Which of the following should be examined when developing documentation integrity projects?
A patient is admitted for chronic obstructive pulmonary disease (COPD) exacerbation. The patient is on 3L of home oxygen and is treated during admission with 3L of
oxygen. The most appropriate action is to
The BEST place for the provider to document a query response is which of the following?
A hospital administrator has hired a clinical documentation integrity (CDI) firm to improve its revenue objectives. The physicians object to this action. How should the firm collaborate with physicians to overcome their objections?
Which factors are important to include when refocusing the primary vision of a clinical documentation integrity (CDI) program?
Besides the physician advisor/champion, who should be included as a key stakeholder in the clinical documentation integrity (CDI) steering committee to promote CDI
initiatives?
The clinical documentation integrity (CDI) manager is reviewing physician benchmarks and notices a low-severity level being measured against average length of stay.
What should the CDI manager keep in mind when discussing this observation with physicians?
When there are comparative contrasting diagnoses supported by clinical criteria, the correct action is to
Which member of the clinical documentation integrity (CDI) team can help provide peer-to-peer level of education on the importance of accurate documentation and
query responses?
An 88-year-old male is admitted with a fever, cough, and leukocytosis. The physician documents admit for probable sepsis due to urinary tract infection (UTI). Antibiotics are started. Three days later, the blood and urine cultures are negative, the patient has
been afebrile since admission, and the white blood count is returning to normal. What documentation clarification is needed to support accurate coding of the record?
A clinical documentation integrity practitioner (CDIP) hired by an internal medicine clinic is creating policies governing written queries. What is an AHIMA best practice for these policies?
Proposed changes to the inpatient prospective payment system (IPPS) take effect on
A physician documented the specific site of the malignancy in the medical record documentation; however, the coder is unable to locate a specific entry in the ICD-10-
CM Alphabetical Index to match the specified diagnosis. Which abbreviation used in the Alphabetical Index will assist the coder in assigning the appropriate diagnosis
code for the specified condition?
A hospital clinical documentation integrity (CDI) director suspects physicians are over-using electronic copy and paste in patient records, a practice that increases the
risk of fraudulent insurance billings. A documentation integrity project may be needed. What is the first step the CDI director should take?
A hospital administrator wants to initiate a clinical documentation integrity (CDI) program and has developed a steering committee to identify performance metrics. The
CDI manager expects to use a case mix index as one of the metrics. Which other metric will need to be measured?
When benchmarking with outside organizations, the clinical documentation integrity practitioner (CDIP) must determine if the organization is benchmarking with which
of the following criteria?
AHIMA suggests which of the following for an organization to consider as physician response rate and agreement rate?
Which of the following criteria for clinical documentation means the content of the record is trustworthy, safe, and yielding the same result when repeated?
A clinical documentation integrity practitioner (CDIP) in an acute care hospital was asked to create new query templates for ICD-10 based on AHIMA and ACDIS
guidelines. What should the multiple-choice query format include?
What type of query may NOT be used in circumstances where only clinical indicators of a condition are present, and the condition/diagnosis has not been documented in
the health record?
Which of the following individuals is the first line of escalation for an unanswered query?
The clinical documentation integrity (CDI) manager reviewed all payer refined-diagnosis related groups (APR-DRG) benchmarking data and has identified potential opportunities for improvement. The manager hopes to develop a work plan to target
severity of illness (SOI)/risk of mortality (ROM) by service line and providers. How can the manager gain more information about this situation?
The clinical documentation integrity practitioner (CDIP) performed a verbal query and then later neglected following up with the provider. How should the CDIP avoid a
compliance risk for this follow up failure according to AHIMA's Guidelines for Achieving a Compliant Query Practice?
A 75-year-old, diabetic patient with a history of osteoporosis, being treated with Fosamax, who sustained a femur fracture after falling down three stairs. The provider's documentation indicates to admit the patient for a traumatic femur fracture and an
orthopedics consult is pending. The clinical documentation integrity practitioner (CDIP) decides to query for a possible link between osteoporosis and the femur fracture. Which of the following is the most compliant query based on the most recent
AHIMA/ACDIS query practice brief?
A patient is admitted due to pneumonia. On day 1, a sputum culture is positive for psuedomonas bacteria. If the physician is queried and agrees that the patient has
pseudomonas pneumonia, this specificity would
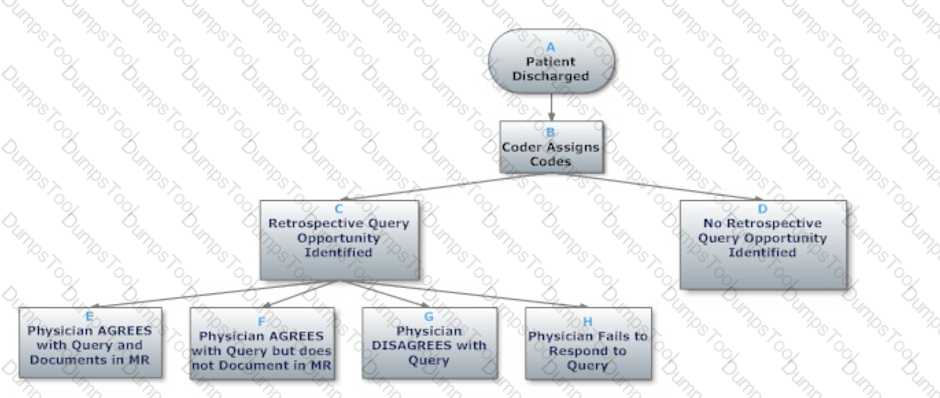
Based on the flowchart below, at what point might the clinical documentation integrity practitioner (CDIP) enlist the help of the physician advisor/champion?
A clinical documentation integrity practitioner (CDIP) is looking for clarity on whether a diagnosis has been "ruled in" or "ruled out". Which type of query is the best option?
A patient was admitted for high fever and pain in umbilical region. During the second day of the hospital stay, the patient stood up to use the restroom and fell on the floor, resulting in a broken chin bone. A physician noted the fall on the second day in
progress note. Which further clarification should be done regarding present on admission (POA) indicator of fall?
In order to best demonstrate the impact of clinical documentation on severity of illness and risk of mortality, which of the following examples is the most effective for
physicians in a hospital?
Automated registration entries that generate erroneous patient identification—possibly leading to patient safety and quality of care issues, enabling fraudulent activity involving patient identity theft, or providing unjustified care for profit—is an example of a potential breach of:
Which of the following sources provide external benchmarks to examine the effectiveness of a facility's clinical documentation program?